Overcoming Denials: The Power of Clinical and Revenue Cycle Teamwork
Claim denials are a big problem in healthcare. They cost a lot of money and create extra work. One main reason is that clinical and revenue cycle teams don’t always work well together. This article shows how teamwork can help reduce denials.
Understanding the Denial Problem
What Are Claim Denials?
Claim denials happen when insurance companies say no to paying for services. This can happen because:
- Authorization Denials: Pre-approvals were not done.
- Medical Necessity Denials: Insurers think the service was not needed.
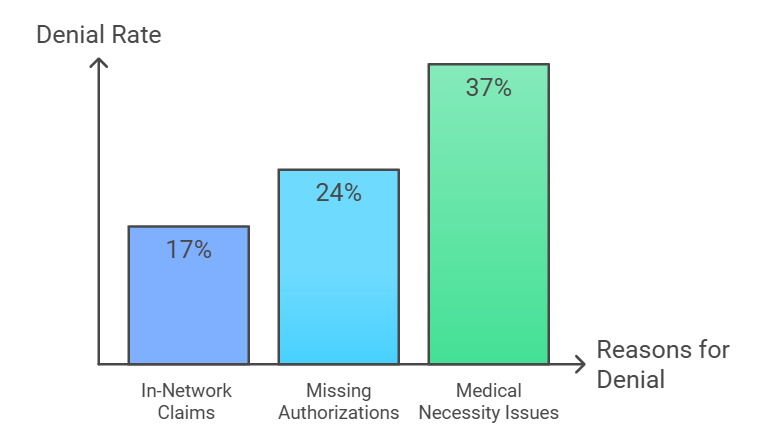
Denial rates are high:
- 17% of in-network claims get denied.
- 24% are due to missing authorizations.
- 37% are due to medical necessity issues.
These denials can cost organizations up to $2 million each year.
The Impact of Denials
Denials hurt healthcare organizations by:
- Losing Money: Providers don’t get paid for services they give.
- Extra Costs: Handling denied claims takes time and resources.
More than 22% of organizations lose a lot of money because of denials. Without a plan to reduce them, these losses will keep growing.
Stop Losing Money on Denied Claims!
Get the expert support you need. Call 949-507-3011 and start improving your claim approvals now!
The Role of Clinical and Revenue Cycle Teams
Clinical Teams
Clinical teams take care of patients and keep records. They write down everything about treatments and outcomes. Accurate records are important because errors or missing info can lead to denials.
For example: If a procedure isn’t recorded right, insurers might say it wasn’t needed. To stop this, clinical teams need to make sure their notes are clear and complete.
Revenue Cycle Teams
Revenue cycle teams handle billing and claims. They need good records from clinical teams to do their job right. If records are wrong:
- Claims might be coded wrong.
- Insurance companies might deny payment.
For claims to be approved, revenue cycle teams need accurate info from clinical teams.
Bridging the Gap: Strategies for Collaboration
Establish Open Communication Channels
Clear communication between clinical and revenue cycle teams is key to reducing denials. Here’s how they can improve communication:
Strategy
Benefits
Set Shared Goals
Align both teams to reduce denial rates.
Track Key Metrics
Use KPIs like first-pass claim approval rates.
Hold Regular Meetings
Discuss denial trends and find solutions together.
Implement Ongoing Education and Training
Training helps both teams understand how their work affects success. Here’s what effective training should include:
- For Clinical Teams: Teach staff how incomplete records lead to denials.
- For Revenue Cycle Teams: Train staff on clinical workflows so they can fix issues quickly.
Cross-training helps both teams see things from each other’s view. This reduces mistakes and improves teamwork.
Leverage Automation Technology
Technology can help reduce errors in records and billing. Here are some tools that make a difference:
Technology can reduce errors and boost efficiency. Useful tools include:
Tool
Function
AI Tools
Create accurate clinical notes in real-time.
Robotic Process Automation (RPA)
Automate billing tasks and reduce errors.
Analytics Tools
Identify patterns and root causes of denials.
Tired of Claim Denials Eating into Your Revenue?
Call us today at 949-507-3011 and discover how Core One Med can help you reduce denials and boost efficiency!
Case Studies and Success Stories
Collaborative Success at a Large Hospital
A hospital was struggling with high denial rates due to poor communication between clinical and revenue cycle teams. Here’s what they did:
Strategies:
- Held regular meetings to review denial trends.
- Set shared goals like reducing denial rates by 20%.
- Trained clinical staff on the financial impact of documentation errors.
Results:
- Denial rates dropped by 25% in one year.
- Appeal times were reduced by 30%.
- The hospital saved over $1.5 million annually.
This shows how teamwork can lead to big financial improvements.
Technology Integration at a Specialty Clinic
A clinic faced high denial rates caused by inconsistent documentation and coding errors. They decided to focus on technology solutions:
Strategies:
- Introduced AI tools for clinical documentation.
- Used RPA for billing tasks to reduce manual errors.
- Analyzed denial patterns with advanced analytics tools.
Results:
- Denial rates dropped by 40% within six months.
- Manual coding errors were reduced by 50%.
- The clinic recovered $500,000 in lost revenue.
This example highlights how technology can improve accuracy and efficiency while reducing costs.
Conclusion
Working together helps clinical and revenue cycle teams reduce claim denials. They need to talk to each other often. They should also have regular training sessions. Using technology can help too. These steps save money and make work easier.
Frustrated by Claim Denials?
We’ve got the solution. Call 949-507-3011 and let Core One Med help you streamline your processes today!









